The Mental Health Imperative.
 In a previous note, I addressed how we may engage with preventing mental illness to improve the health of populations. Since then, I have become ever more convinced that mental health represents a too-often neglected component of population health, meriting far more attention than it currently receives. Reflecting on this topic, and thinking about how we can better elevate the visibility of mental disorders, I would like to use today’s note to suggest three straightforward reasons why mental health is of critical importance to public health, and why it is imperative that we tackle the problem of mental illness with as much energy and innovation as we apply to other, more widely addressed population health concerns. There are many other reasons, of course, but I thought I would focus on three, just to make the case simply, and hopefully usefully.
In a previous note, I addressed how we may engage with preventing mental illness to improve the health of populations. Since then, I have become ever more convinced that mental health represents a too-often neglected component of population health, meriting far more attention than it currently receives. Reflecting on this topic, and thinking about how we can better elevate the visibility of mental disorders, I would like to use today’s note to suggest three straightforward reasons why mental health is of critical importance to public health, and why it is imperative that we tackle the problem of mental illness with as much energy and innovation as we apply to other, more widely addressed population health concerns. There are many other reasons, of course, but I thought I would focus on three, just to make the case simply, and hopefully usefully.
1. Mental disorders impose a high, though likely under-measured, burden
Mental illness accounts for almost 15 percent of the total global burden of disease. The World Health Organization’s World Mental Health Survey Initiative, which carries out household, in-person interviews across the Americas, the Middle East, Africa, and Asia, found that the prevalence of mental disorders varies widely across different areas of the world, with the US having the highest reported past-year prevalence of any disorder, at about 26 percent.
The category of “mental illness” is broad, encompassing everything from severe disorders such as schizophrenia or bipolar disorder, to substance abuse, to the more common conditions of depression and anxiety. Depression, in particular, is among the most widespread of these challenges, and often co-occurs with other serious disorders. The WHO has projected that depression will be the leading cause of global disease burden by 2030. An estimated 350 million people are currently affected by the condition, the majority of whom are women.
Th

Dingfelder SF. Stigma: Alive and Well. Monitor on Psychology. 2009; 40(6): 56.
For these reasons, mental disorders represent a high—though likely underestimated—burden of illness and disability, both domestically and globally. This, to my mind, makes a prima facie argument for the importance of mental health to the health of populations, and for raising mental health’s status as a pressing public health concern.
2. Mental disorders are sensitive to contemporary social conditions
The drivers of mental disorders include a complex mix of contextual and individual factors, including environment, genetics, and early-life childhood experiences. Mental illness may be particularly sensitive—relative to physical illness—to these conditions. Consider the link between income and mental health. We know that income is associated with many highly prevalent and common mood-anxiety disorders. By way of one illustration, from 2009 to 2013, 8.7 percent of individuals with annual incomes lower than the federal poverty line reported “serious psychological distress,” compared with just 1.2 percent of individuals with annual incomes at, or over, four times higher than the poverty line (Figure 2).
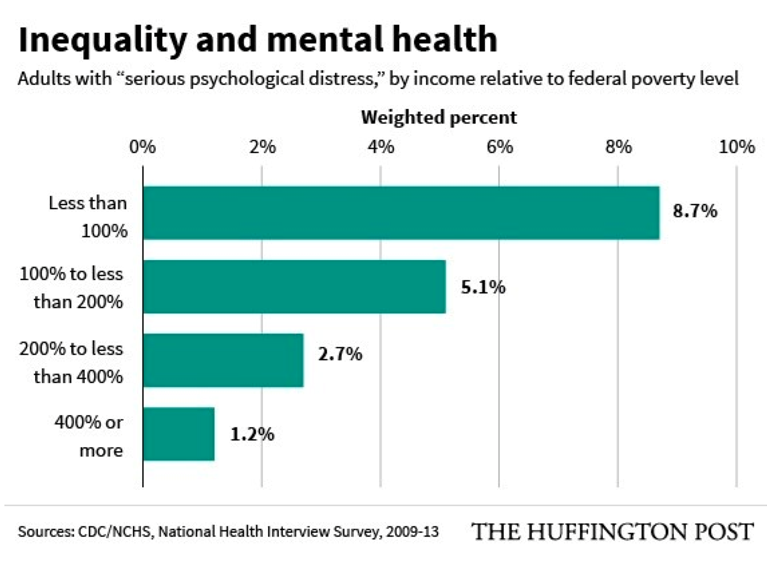
Cohn J. Mental Illness is a Much Bigger Problem for the Poor, New Study Shows. The Huffington Post. May 28, 2015. http://www.huffingtonpost.com/2015/05/28/mental-health-coverage_n_7456106.html Accessed February 14, 2017.
As I have pointed out in previous notes, several other conditions, such as discrimination against LGBT populations and racial minorities, can be associated with depression and other mental illnesses. This is the case among individuals who experience discrimination as both a direct stressor, and, more indirectly, through difficulty accessing care. On an interpersonal level, sexual violence, one of the most traumatic events a person can experience, is associated with a high conditional risk of subsequent mental illness.
These associations suggest that mental health is, in a sense, a bellwether for the times, reflecting prevailing conditions, with the occurrence of adversity fueling mental illness rates. A concrete illustration of this can be found in the eastern Mediterranean region, where there was a nearly 11 percent increase in disability-adjusted life-years (DALYs) between 1990 and 2013. Depression and anxiety disorders accounted for the largest proportion of DALYs, with Palestine seeing the greatest burden in this area. This increase may be related to ongoing turmoil in the region—experiencing or witnessing violence and other traumatic events is strongly associated with poor mental health outcomes, particularly post-traumatic stress disorder (PTSD) and depression. Other types of traumatic events that often lead to an increased burden of mental disorder include exposure to natural disasters. Such disasters are increasingly widespread throughout the world, partially due to changes in climate.
The degree to which the proximal foundational determinants of well-being influence mental health suggests the need for renewed focus on mental health, particularly as it is shaped during times of adversity. This is very much the coin of public health’s realm; improving these determinants can result in improvement in population mental health. This agitates for public health’s engagement with foundational conditions, towards the goal of improving the health of populations.
3. Early childhood is a critical period for mental health, presenting opportunities for prevention
Mental illness tends to start earlier than other chronic diseases, and the burden of mental illness among the young is substantial. As of 2011, as many as half of all US children and adolescents met diagnostic criteria for at least one mental health disorder by the age of 18 (Figure 3). Importantly, mental disorders increase the risk of other disorders over the lifecourse. In general, individuals with mental disorders have higher mortality rates than their peers, which are attributable to co-occurring physical health problems such as diabetes, cardiovascular disease, and HIV. Mental disorders present a particular hazard through their association with suicide, which accounts for more than 800,000 deaths per year globally.
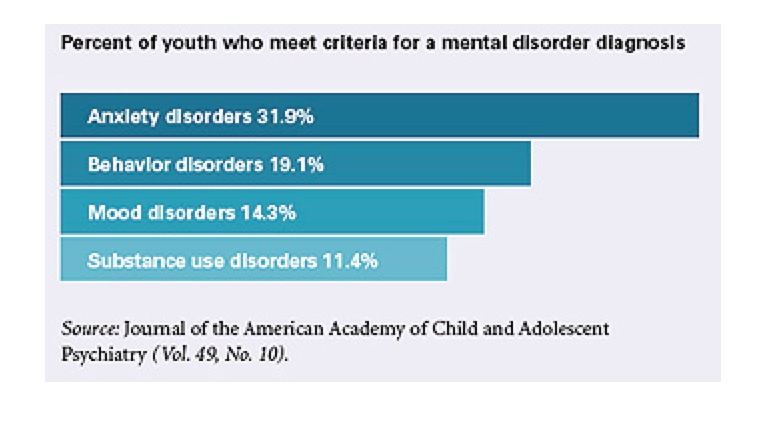
New data on mental illness among US youth. Monitor on Psychology. 2011; 42(2): 10.
Th
Mental health has come into focus in recent years as integral to the overall picture of population health. In the US, increased media coverage has called attention to mental health, partially due to suicide’s role in lowering life expectancy among middle-aged white Americans. The Boston Globe Spotlight Team’s series, “The Desperate and the Dead,” is one example of the power of reporting to convey how our legal, political, and health systems often fail the mentally ill. Here at SPH, through our events, our scholarship, and the advocacy of our students and alumni, we have been consistent in our position that mental health is just as important as physical health, and no less worthy of attention and, most importantly, prevention. We aspire to do ever more to promote this perspective, towards a world where we, as much as possible, prevent and mitigate the consequences of mental illness in populations.
I hope everyone has a terrific week. Until next week.
Warm regards,
Sandro
Sandro Galea, MD, DrPH
Dean and Robert A. Knox Professor, Boston University School of Public Health
Twitter: @sandrogalea
Acknowledgement: I am grateful to Laura Sampson and Eric DelGizzo for their contributions to this Dean’s Note.
Previous Dean’s Notes are archived at: /sph/tag/deans-note/
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.