Racism and the Health of the Public.
 Before discussing today’s topic, I wanted to pause for a moment to reflect, with sadness, on the devastation wrought by the earthquake in Nepal last week. As of this writing, more than 6,000 people have died in the earthquake that has shaken Katmandu and the entire country, with the death toll expected to rise steeply. I have spent a substantial portion of my academic career studying the consequences of large-scale traumatic events, gaining, through that academic journey, an appreciation of the scale of the consequences of these events. While the death toll is what typically reaches the news pages, hidden behind the front page are always stories of remarkable human resilience and endurance. Away from the cameras, however, will be a tremendous health toll, much of it in the form of poor mental health in the population for years after the event. The Nepalese population will slowly emerge from this event, even as a new normal takes shape that includes memories of the disaster, and those who bear its memories, for decades to come. Meanwhile, our heart goes out to all affected by the disaster, and our thoughts are with the local and global Nepalese community.
Before discussing today’s topic, I wanted to pause for a moment to reflect, with sadness, on the devastation wrought by the earthquake in Nepal last week. As of this writing, more than 6,000 people have died in the earthquake that has shaken Katmandu and the entire country, with the death toll expected to rise steeply. I have spent a substantial portion of my academic career studying the consequences of large-scale traumatic events, gaining, through that academic journey, an appreciation of the scale of the consequences of these events. While the death toll is what typically reaches the news pages, hidden behind the front page are always stories of remarkable human resilience and endurance. Away from the cameras, however, will be a tremendous health toll, much of it in the form of poor mental health in the population for years after the event. The Nepalese population will slowly emerge from this event, even as a new normal takes shape that includes memories of the disaster, and those who bear its memories, for decades to come. Meanwhile, our heart goes out to all affected by the disaster, and our thoughts are with the local and global Nepalese community.
Racism and the Health of the Public
Moving on to the topic at hand, over the past 12 months, the list of reported incidents in which police have harmed unarmed black men seems inexhaustible. Earlier incidents involving Amadiou Diallo and Sean Bell have been followed, in the past year alone, by Michael Brown, Walter Scott, Eric Garner, and most recently Freddie Gray.
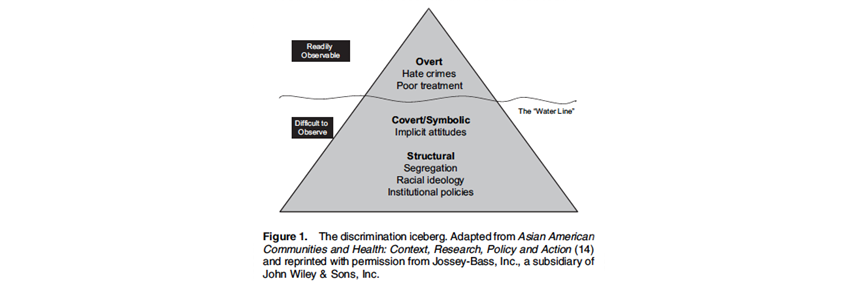
These events have been accompanied by an outpouring of anguished civic protest, and by commentary that has well noted how racism in US life continues to loom large and to shape our experiences and interactions. Seen through this lens, these instances of police-inflicted injury are merely the tip of the iceberg, where racism reaches a tragic end. These events do not, however, capture the extent of racist social interactions and structures that shape the experiences of millions beyond those whose plight reaches the news. In a particularly powerful piece, New York City Commissioner of Health and Mental Hygiene Mary Bassett commented on #BlackLivesMatter and the implications of the recent, very public, demonstrations of anger around racial divides for the medical and public health communities.
Informed by this discussion, how should we, in the academic public health community, think about racism and the health of populations, and about our responsibility to tackle this issue towards a healthier public?
While there are many ways in which we can consider the impact of racism on health, it may be useful to think of racism’s impact on two levels: interpersonal or individual racism, and structural or institutional racism. There is ample evidence of the impact of racism on health in both domains, and the iceberg metaphor serves to illustrate the distinction between the more readily observable (i.e. interpersonal) versus the more difficult to observe (i.e. structural) dimensions of racism [see Figure 1]. Informing our understanding of how discrimination, both interpersonal and structural, can contribute to health inequities and how to test such hypotheses, Nancy Krieger provides a useful conceptual model [see Figure 2].
Gee G. C., Ro A., Shariff-Marco S., & Chae D. (2009). Racial discrimination and health among Asian Americans: Evidence, assessment, and directions for future research. Epidemiol Rev, 31(1), 130-151. http://www.ncbi.nlm.nih.gov/pubmed/19805401
圣
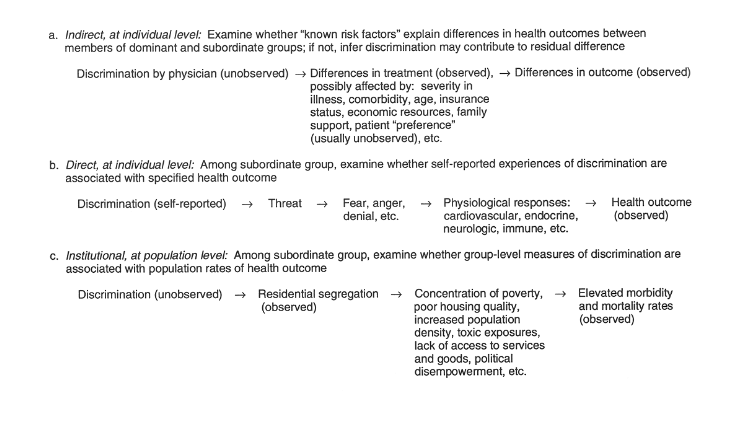
Krieger N. (1999). Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv, 29(2), 295-352; http://www.ncbi.nlm.nih.gov/pubmed/10379455
莫
What, then, is our responsibility, as members of an academic school of public health community, to engage this issue? I would argue that we have a responsibility on four levels.
First, we are, at core, engaged citizens of our local and global communities. In that capacity, some of us may choose to participate in public shows of support with affected communities, ensuring that this issue rises to the top of the public conversation, and stays there. Peaceful public statements of concern about a pressing social issue always have a place in an open society, and our responsibility as members of society is not obviated by our membership in our academic community.
Second, we are members of a university community. Generation of knowledge is the primary responsibility of universities, and the generation of relevant knowledge that can help inform acute social needs is the particular remit of professional schools. This nudges us towards a scholarship of consequence, where, in this particular instance, we aim to shed light on the root causes of the racial divides that are informing the public debates of the moment, and of the link between racism and the health of the public. This of course suggests a concern with prioritizing our research questions, focusing, as I have argued, on what matters most, and orienting our scholarship towards areas of inquiry that tackle the foundational drivers of population health.
Third, we are charged with transmitting knowledge to students, with education that both teaches the foundations of our field and prepares students to engage in evolving issues of contemporary public health importance. That calls for an education that is dynamic and reflexive, but also an educational environment that encourages and respects sharing of ideas, towards the goals of engendering mutual understanding and identifying solutions grounded in diversity of experience, opinion, and perspective. It is simply not enough to accept that our educational program is rooted in concern around issues of disparities; we need to engage in hard, sometimes uncomfortable discussions about these issues in order to understand one another and our potentially different perspectives on challenging issues. As a school, we are working towards creating the forums for such discussions and embedding formal education on this in our program.
Fourth, translation of our ideas is one of our core responsibilities as a school of public health. Insofar as public health rests on the generation of conditions that make people healthy, and insofar as those conditions depend on the introduction of health in all policies and in all sectors, we need to work towards a health conversation that extends well beyond our academic walls. We need to engage with the public conversation that aims to inform and influence how we understand racism and its consequences, to better understand the health consequences of racism, the pathways that explain these links, and how these links may be broken. Needless to say, racism and hate of any kind are intolerable separate from their health consequences. But health, as a universal aspiration, can serve as a clarifying lens for action, as one more tool to elevate the import of these issues in a public conversation that in the end aspires to create a society that indeed makes populations healthy.
I aspire indeed to meeting these responsibilities together. Until next week.
Warm regards,
Sandro
Sandro Galea, MD, DrPH
Dean and Professor, Boston University School of Public Health
@sandrogalea
Acknowledgement: I would like to acknowledge the help of Gregory Cohen, MSW on this Dean’s Note and the comments of Associate Dean for Education Lisa Sullivan that helped shape my thinking in this Note.
Previous Dean’s Notes are archived at: /sph/category/news/deans-notes/