Incarceration and the Health of Populations.
 Public health as an organized enterprise emerged from a concern with living conditions in the mid-nineteenth century. It was a beginning that foreshadowed public health’s long engagement with social forces that influence the health of populations. However, there is also a range of issues that public health has not engaged with as forcefully as it perhaps might, given the public health consequences of these issues. I have, in a previous Dean’s Note, commented on firearms and their impact on the health of the public. I see firearms as a preventable epidemic, and one that should, and can, be a part of the public health conversation as we aim to identify areas where we can have impact to improve population health. Here I write briefly about another such issue, overlooked in my estimation by public health relative to the impact it has on the health of the public: incarceration. While this is an issue that has resonance for population health worldwide, I limit these comments to the US, animated by the challenge this issue poses for health at home.
Public health as an organized enterprise emerged from a concern with living conditions in the mid-nineteenth century. It was a beginning that foreshadowed public health’s long engagement with social forces that influence the health of populations. However, there is also a range of issues that public health has not engaged with as forcefully as it perhaps might, given the public health consequences of these issues. I have, in a previous Dean’s Note, commented on firearms and their impact on the health of the public. I see firearms as a preventable epidemic, and one that should, and can, be a part of the public health conversation as we aim to identify areas where we can have impact to improve population health. Here I write briefly about another such issue, overlooked in my estimation by public health relative to the impact it has on the health of the public: incarceration. While this is an issue that has resonance for population health worldwide, I limit these comments to the US, animated by the challenge this issue poses for health at home.
In 2012, there were nearly 1.6 million prisoners in the US state and federal prison population [see figure 1]. The incarceration rate in the US (716 per 100,000 people) is higher than any other country in the world, and about five times higher than the median worldwide (144 per 100,000).
![[Figure 1] Source: http://sentencingproject.org/doc/publications/inc_Trends_in_Corrections_Fact_sheet.pdf](/sph/files/2015/03/figure1.png)
Source: http://sentencingproject.org/doc/publications/inc_Trends_in_Corrections_Fact_sheet.pdf
Why does the US have such astoundingly high incarceration rates? Instrumentally, much of the rise of the prison population in the US appears to be largely a result of the Rockefeller Drug Laws, implemented in 1973 in New York State, which targeted drug offenders and took root as a model for national policy. Indeed, the incarceration rate of drug offenders rose explosively over the following three decades, as did the proportion of drug-related prison commitments. Perhaps at a more foundational level, we have as a society accepted that incarceration and retribution are acceptable, maybe even desirable, parts of our armamentarium to deal with fears about violence, rather than choosing other alternative forms of punishment or conflict resolution that minimize the recourse to incarceration. The role of social norms, and how they may influence our broader health conversation, shall be the subject of another Dean’s Note.
Why should public health care about incarceration? There is, unfortunately, ample evidence that incarceration is associated with health of populations, both directly—that is, for those who are incarcerated—and indirectly, for their families and communities.
圣
![[Figure 2] Source: http://www.law.uchicago.edu/files/file/harcourt_institutionalization_final.pdf](/sph/files/2015/03/figure2.png)
Source: http://www.law.uchicago.edu/files/file/harcourt_institutionalization_final.pdf
This suggests that many individuals in need of mental health care are instead being diverted to our prison systems. Although prisoners are the only US citizens with a constitutional right to health care, they often face delays in access to care, restrictive medication formularies, a lack of acute care options, and understaffing of specialty care medical providers. Female prisoners face particular challenges in getting care that is timely and appropriate. Substance use disorders are, predictably, also quite high among those incarcerated, and of the estimated 70 percent to 85 percent of prisoners in need of treatment, only 10 percent receive such services.
Th
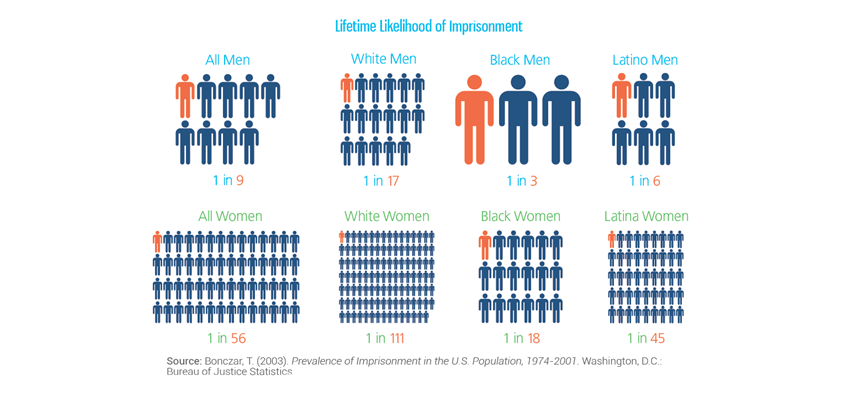
Separately, any discussion of the effects of incarceration must recognize that the burdens and consequences of incarceration are borne unevenly across US society, with minority populations being vastly and disproportionately affected by incarceration. Mass incarceration and its effects are wrought unequally on blacks and Hispanics [see figure 3]. To concertize this, among children born in 1990, 1 in 25 whites and 1 in 4 blacks had a parent imprisoned by age 14, an increase in magnitude and racial disparity compared with those born in 1978.
Source: http://sentencingproject.org/doc/publications/inc_Trends_in_Corrections_Fact_sheet.pdf
In a previous Dean’s Note, I commented on the health consequences of discrimination and will in future notes comment on the pervasive influence, as I see it, of racial/ethnic marginalization on population health in the US. However, for the purposes of this comment, I note that this extreme disproportion, by a factor of six among men, of black–white differences in incarceration represents a level of systematic marginalization and concentration of adversities faced by minority communities that represents on the biggest threats to the production of health throughout the country.
哈
I hope everyone has a terrific week. Until next week.
Warm regards,
Sandro
Sandro Galea, MD, DrPH
Dean and Professor, Boston University School of Public Health
@sandrogalea