Center for
regenerative medicine
Discover CReM
About CReM
Human health and development depend on dynamic networks of physical, and functional, interactions between proteins. 然而,这些网络的细节——它们是如何形成的,又是如何 they function – are largely unknown.
Upcoming Seminars
Martin Tristani-Firouzi, MD
Investigator, Nora Eccles Harrison Cardiovascular Research & Training Institute
Professor of Pediatrics
H.A. and Edna Benning Presidential Chair
Co-Director of the Center for Genomic Medicine
University of Utah
Special Guests
Hao Zhu, MD
The Nancy B. and Jake L. Hamon Distinguished Chair in Therapeutic Oncology Research
Children’s Medical Center Research Institute
University of Texas Southwestern Medical Center
Marianne Bronner, PhD
Edward B. Lewis Professor of Biology
Director of the Beckman Institute
Division of Biology and Biologic Engineering
California Institute of Technology
We Are Hiring
Make a Donation
Financial Support
Research Programs
CReM in the News!

What’s the secret to living to 100? Centenarian stem cells could offer clues
A bank of cells from people more than 100 years old gives scientists a new resource for studying longevity
- News

- News
Linkup aims to drive research into pulmonary fibrosis, a disease with no cure | Click here to read
The Brink | By Andrew Thurston | Photos by Cydney Scott
October 17, 2024
- News

- News

- Publications
Click here to read
Todd W. Dowrey, Samuel F. Cranston, Nicholas Skvir, Yvonne Lok, Brian Gould, Bradley Petrowitz, Daniel Villar, Jidong Shan, Marianne James, Mark Dodge, Anna C. Belkina, Richard M. Giadone, Sofiya Milman, Paola Sebastiani, Thomas T. Perls, Stacy L. Anderson, George J. Murphy.
- Publications
Publication from the Murphy Lab: Click here to read the article.
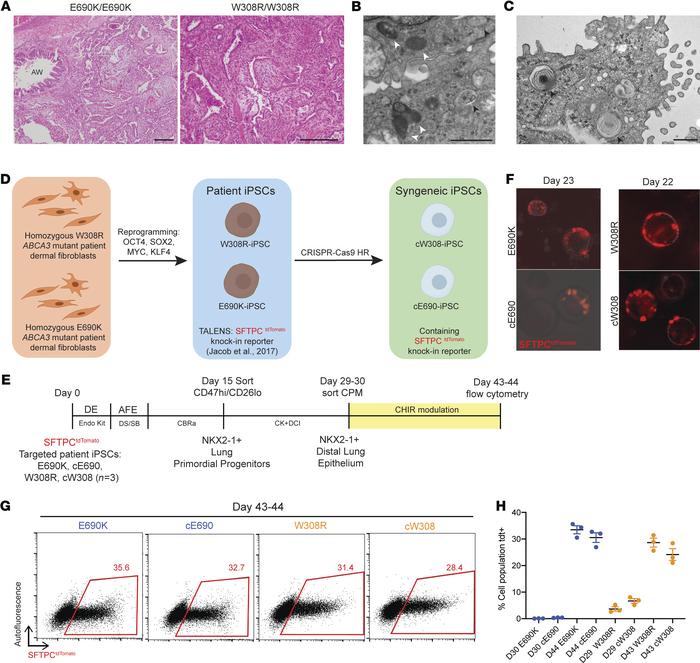
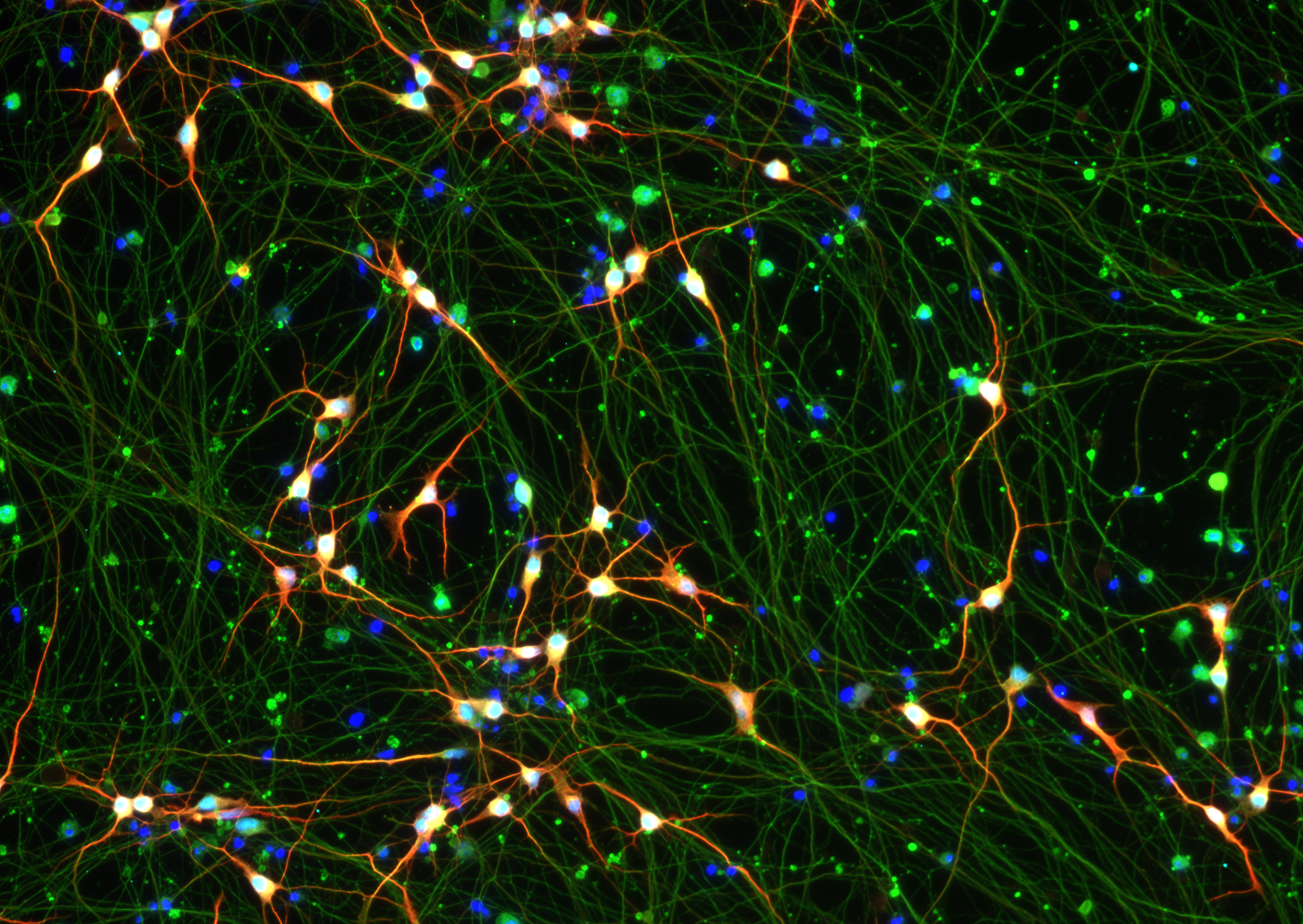
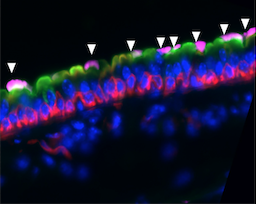
Alveolar epithelial type I cells (AT1s) line the gas exchange barrier of the distal lung and have been historically challenging to isolate or maintain in cell culture. Here, we engineer a human in vitro AT1 model system via directed differentiation of induced pluripotent stem cells (iPSCs). We use primary adult AT1 global transcriptomes to suggest benchmarks and pathways, such as Hippo-LATS-YAP/TAZ signaling, enriched in these cells. Next, we generate iPSC-derived alveolar epithelial type II cells (AT2s) and find that nuclear YAP signaling is sufficient to promote a broad transcriptomic shift from AT2 to AT1 gene programs. The resulting cells express a molecular, morphologic, and functional phenotype reminiscent of human AT1 cells, including the capacity to form a flat epithelial barrier producing characteristic extracellular matrix molecules and secreted ligands. Our results provide an in vitro model of human alveolar epithelial differentiation and a potential source of human AT1s.
- Publications
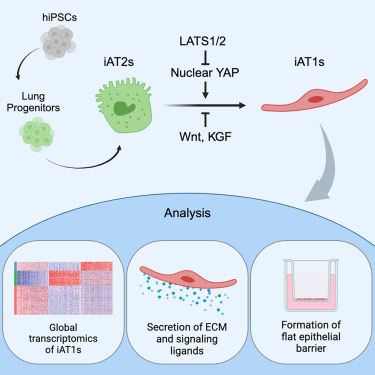
Kotton and colleagues generate human alveolar epithelial type I cells (AT1s) from induced pluripotent stem cells (iPSCs). The resulting cells can be grown as 3D organoids or in 2D air-liquid interface cultures, displaying many of the molecular, morphologic, and functional phenotypes of primary AT1s.
- Funding

A team of researchers led by Darrell N. Kotton, MD, the David C. Seldin Professor of Medicine, has been awarded a five-year, $14 million grant from the NIH’s National Heart, Lung, and Blood Institute (NHLBI) for their research, “Developing Pluripotent Stem Cells to Model and Treat Lung Disease.” The new award will fund an integrated, multi-investigator program project grant where four interacting labs headed by four physician-scientists, all located in the Center for Regenerative Medicine (CReM) of Boston University and Boston Medical Center, will develop next generation stem cell-based therapies for currently incurable genetic lung diseases affecting children and adults, including childhood and adult interstitial lung diseases, an inherited form of emphysema, cystic fibrosis and primary ciliary dyskinesia.